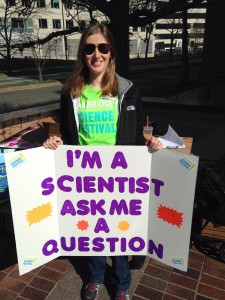
What I’m Reading: The Radium Girls
My favorite types of books are nonfiction, specifically the history of science. It’s the nature of science that so many discoveries and innovations throughout history shaped not only the eras in which they originated, but continue to shape the society of their futures. I also find it so compelling to discover the story of someone who lived and died, contributing to a scientific advance that has had an impact on us all, but whose name has been outlived by their deeds. With this in mind, it is probably not surprising that The Radium Girls: The Dark Story of America’s Shining Women by Kate Moore fits squarely into my literary comfort zone, and that I loved it.
Starting right after World War I, The Radium Girls chronicles the rise of radium as a wonder element, incorporated into untold numbers of beauty and household products, as well as used industrially for its ability to glow in the dark. This was an era in which a glow-in-the-dark wrist watch was an extremely sought-after item, and companies like the United States Radium Corporation and the Radium Dial Company sprung up to cash in on the radium craze.
My copy of The Radium Girls. Photo by Erin Podolak.
Hundreds of young women, some barely into their teens, came to work at these companies because they offered well-paying jobs at a time when families were struggling. Young women who could work would do so to help support their families in the years before they established families of their own or to provide themselves with spending money. At the time, while some scientists were just discovering that radium could be extremely dangerous, the public image of the substance was that it was beneficial and couldn’t possibly be harmful.
A well-paying job with other young women in a joyful and convivial atmosphere, working with a healthful wonder substance that had the added bonus of making your clothes and hair glow-in-the-dark? It was an opportunity few women could pass up. So women flocked to the factories, spending every day sitting in a studio painting watch dials with luminescent radium paint. To paint the small numbers on the dials, the women used a technique called “lip pointing” –twirling their paint brush in their mouth between highlighting each number to make a fine point, ingesting traces of the radium paint each time they did so.
Within a few years, the “dream job” bubble would burst as women started suffering from mystery illnesses: tooth decay, mouth sores that wouldn’t heal, pain in their feet, their backs, their hips, low blood cell counts, sarcomas, and even bones that simply crumbled at the touch. Ultimately, scores of women would die of these illnesses, many long before the women and their doctors were able to figure out that it was exposure to the radium that was harming them.
Radium was still new enough that its negative effects were poorly understood, and illnesses like the dial-painters had never been seen before. Companies profiting from radium and the girls’ work had every interest in preserving radium’s healthful image and their own finances. The companies would go to excessive lengths to avoid taking responsibility for any of the women harmed by the radium in their studios. Moore’s book tells the story of these women, as they struggled to make sense of what could have harmed them, never dreaming it could be their employers. She notes their dramatic turns from victims to advocates as they discovered their own poisoning, fighting until the end to make sure that the companies were forced to do the right thing for their workers.
One of the things about the Radium Girls that I loved was the connection to the women that Moore clearly feels. She cares about their stories, protecting them, preserving them, and telling it right. Moore writes beautifully, with sentences that lingered in my mind, hammering home the point that she is trying to make. For example, Moore describes the exhumation of a radium worker years after her death, while seeking evidence to bolster the evidence that radium could kill:
“When they checked the x-ray film, days later, there was Mollie’s message from beyond the grave. She had been trying to speak for so long-now, at last, there was someone listening. Her bones made white pictures on the ebony film. Her vertebrae glowed in the vertical white lights, like a regiment of matches slowing burning into black. They looked like rows of shining dial painters walking home from work. The pictures of her skull, meanwhile, with her jawbone missing, make her mouth stretch unnaturally wide, as though she was screaming-screaming for justice through all these years.” The Radium Girls, page 194.
It’s a passage that I read and re-read, and I think it showcases how Moore writes. It is captivating and hard-hitting, playing up the facts and their resonance at the same time.
The book shines a light on the misdeeds at the dial painting plants in Newark and Orange, New Jersey and in Ottowa, Illinois. Having grown up in New Jersey, the story of the dial painters struck a chord with me. But the plight of the women in these cities is a story that is altogether engaging and compelling. At the time, radium sickness wasn’t even defined, but the women fought to make their illnesses recognized by the government. They went on to challenge the companies, even forcing changes to worker’s compensation rules, and saving countless lives by exposing radium for the dangerous substance we all now know it to be.
The amount of deceit on the part of the companies made my blood boil with the injustice of it all. I think being a young woman, I could relate to the idea that young women would simply believe their bosses when they said they had their best interest at heart. I think that was a lesson that I learned the hard way early on in my career, that if something seems too good to be true, you have to wonder where the good fortune is coming from and question the motivations behind it. The women never considered the possibility that they were being lied to, that their very lives were worth nothing to the companies compared to their bottom line.
It also gives a new (to me) perspective on corporate misdeeds, how far some people might go to earn a buck, the lies that might be told, and the people that might be harmed. The timeline of events in the book is perhaps the most damning part of the story, because it shows without a doubt how, if the companies and individuals who knew that radium was harmful had owned up to it as soon as they knew, so many lives could have been spared, so much suffering avoided.
In the end, the idea that it was all only for the money, only about profits, just leaves the whole story tinged with sadness, because it does not provide a satisfying answer to the question of why, why would anyone knowingly do this to another human being. “For money” is an answer that is shockingly inadequate in the context of all that these women suffered, all that they were deprived of by these companies.
The Radium Girls is a story that will stay with me for a long time. This story is a piece of science history, as the mystery of radium and what it could do was untangled. It is a piece of American history as the workers compensation laws were rewritten and laws put in place to protect workers. And it is a piece of women’s history as these girls banded together to take on powerful companies in a David and Goliath struggle to do what was right. It’s a fascinating and sobering story, and I wholeheartedly recommend it.
Science Train at the Cambridge Science Festival
Living in Boston affords me direct access to a vibrant scientific community. Just across the river in Cambridge you can find amazing universities and research centers alongside pharmaceutical companies just about everywhere you look. It’s perhaps not surprising that this environment is also home to a lively, 10 day festival that brings hundreds of events around “science” writ large to the Cambridge community.
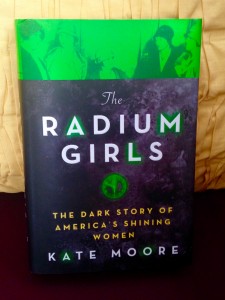
I’m not really a scientist, but I was pretty proud of my posters. Photo by Brian J. Abraham.
Science festivals are a great place to put science communication into practice. This year, I got involved by organizing a Boston version of the Science Train. On Saturday, April 15, small groups of scientists donned their lime green volunteer T-shirts, picked up posters reading “I’m a scientist, ask me a question” and jumped on the T (the Boston/Cambridge subway) to go where the people are and interact with them in a space where we knew they’d be anyway. Bringing science to the public like this isn’t an original idea; we were inspired to do this for the Cambridge Science Festival after hearing about previous Science Train successes in New York. By adapting the idea to run in concert with the Cambridge Science Festival, the Science Train not only served as outreach but was also promoting the festival and the broader selection of science events taking place in Cambridge.
The Cambridge Science Festival, which claims to be the first festival of its kind in the United States, includes a variety of events that offer something for people of all ages. From the festival’s website: “The Cambridge Science Festival offers a wide range of STEAM [Science/Technology/Engineering/Arts/Mathematics]-related activities – lectures, debates, exhibitions, concerts, plays, workshops, etc. – over ten days at a variety of locations [across Greater Boston]. Modeled on art, music, and movie festivals, the Cambridge Science Festival makes STEAM part of the wider culture by illuminating the richness of scientific inquiry and the excitement of discovery.”
Organizing the Science Train mostly entailed sending a lot of emails. It was important that the MBTA know what we were doing, we had to work with the Cambridge Science Festival to synchronize message and branding, and we had to recruit volunteers for the Science Train itself so that we’d get enough to make it a success. We found post-doc associations like the one at MIT to be particularly helpful for recruiting volunteers who were willing to ride the T with us. I also worked to divide the volunteers into shifts and small groups, making sure that there were a variety of scientific backgrounds on each of the teams to cover what was sure to be an array of questions that could come up.

Science Train volunteers. Photo by Erin Podolak.
The volunteers came back saying the Science Train was a worthwhile activity, but that trying to figure out the best way to approach people could be a little awkward. The red line, which runs through Cambridge itself, tends to serve a more science-minded crowd simply because it runs beneath most of the universities and research areas. Other train lines like the orange line cater to groups of people that probably have less exposure to science and scientists on a regular basis. The scientists on the red line seemed to have an easier time initiating conversations, and my explanation is that people on the red line were more comfortable actually asking questions and/or jumping into a conversation with a scientist.
For the most part, the volunteers reported that the questions were things they were able to answer. However, in some groups where there wasn’t a scientist of a particular specialty, it could be hard to answer what was asked (like a biologist being asked a question about the boiling point of peanut butter). A few volunteers did get a question or two that veered into awkward territory, like personal health questions, which prompted them to explain they weren’t medical doctors. One groups of volunteers was also asked about the existence of God and what their thoughts on religion are, which we’re told got a little bit uncomfortable. Some volunteers also mentioned that some people took the sign “I’m a scientist, ask me a question” as a challenge, purposely trying to stump the volunteers rather than have a conversation. We might word the signs differently in the future, but, by and large, we met our goal because the scientists were able to interact with people about science in a place where they already are, bringing science right to them and making science (and scientists) seem a little more approachable.

Volunteer Scientists ready to ride the Science Train. Photo by Erin Podolak.
I think activities like this can be hard to execute well, but they can be really successful if you get enough buy-in from excited volunteers and the powers-that-be. It’s definitely important to know your audience and understand what you might be getting yourself into. This is the kind of activity that might be most successful if there is at least one person per group who is really comfortable and confident in their science communication abilities. An activity like the Science Train isn’t for the timid. Without a guide or examples to follow, it might be really challenging to use it to learn how to do science communication. Of course, when asking for volunteers whom you haven’t met, it can be particularly difficult to find the right mix of people who are going to be successful at sharing science in this format.
I believe strongly that communities benefit from in-person engagement with science and scientists. That said, not all engagement works or is a good idea. The Science Train definitely worked, but getting to know the teams of volunteers in advance and designing different posters are things that I’ll look to tweak in the future. I’m glad I had an opportunity to volunteer for the Cambridge Science Festival and run the Science Train. Not being a scientist myself, I think organizing this event was a great way to help make community/scientist engagement a reality.
Thank you to all the volunteer scientists who spend their Saturday on the Science Train, here’s to more community science engagement in the future.
AAAS 2017 Conference Recap

The program book for the 2017 AAAS conference. Photo by me.
This year, the American Association for the Advancement of Science (AAAS) held it’s annual conference in my neck of the woods (Boston) so I was able to take a few days away from the office to attend. In the realm of conferences that someone in my field might consider going to, AAAS always stands out because it isn’t strictly a communication conference, and it isn’t strictly a science conference – it’s definitely both, with a generous dose of science policy thrown in for good measure. For its range of content AAAS attracts a very eclectic group of attendees. Anecdotally, I think the conference caters a lot to young people, but there are plenty of mid-career and established people who attend as well.
This was my third AAAS conference, and I think the value of science communication is becoming more and more apparent because it has taken an increasingly important place in the conference line up. Thursday (February 16, 2017) the first day of sessions, I attended the communicating science seminar, which was a lineup of three different panel talks the topics of which were: “Who’s your audience?,” “Scientist motivations, support, and challenges for public engagement,” and “The online scientist: social media and public engagement.” I think all of these sessions were sculpted to appeal to scientists more than science writers but there was a lot to get out of them as a science writer.
A few of my key take aways or sound bites from the communicating science seminar are:
- Look for opportunities to inject science communication into events and programs that already exist, ie: setting up a hands on science booth at a local fair, to bring science into the fabric of a community.
- Policy is shaped by the relationship between science, the decision makers, and the public. If the public doesn’t understand or doesn’t like the science, the public pressure on the decision-maker to choose an option not supported by the science can be great – this is why having strong public engagement and understanding of science is so important.
- There is a difference between simply pushing out information and engaging with people, getting them to feel invested in the science by building a relationship.
- Most organizations are designed with a top-down power structure, but the public often isn’t looking for top-down lectures from scientists. Adult-to-adult conversations can go a long way toward making people feel respected and thus willing to listen to what you have to say.
- Try to avoid preconceptions about where people are starting from in their scientific understanding, and acknowledge that sometimes you are not the best person to lead a specific conversation or event. It can be incredibly valuable to facilitate the leadership of others by helping to clear their path.
- You can step out of the role of “the expert” without abandoning your expertise. This looks like having a conversation instead of a lecture. It includes listening to people as well as sharing what you know.
- Remember to read the room and consider the personal dynamics to gauge what type of communication is likely to provide the biggest rewards.
- Often scientists [and communicators] think that informing the public is the goal, but perhaps the goal could be to help the public identify the scientific information that is valuable and useful to them. This might change the relationship people have with science and scientists.
- Two of the most common barriers to science communication and outreach for scientists are time and a lack of institutional buy-in that engaging the public is a part of the job rather than a side interest. The ideal scenario is one in which science communication activities are seen as helpful to one’s career as a scientist.
- People enjoy being told a story, it is often easier and more like science to provide just the facts but for the public facts need framing. Giving the facts context can go a long way toward communicating their value.
Overall Thursday brought a series of interesting conversations, with a great lineup of speakers who brought a nice array of points of view to the table. There were a lot of scientists in the room (they did an informal poll by show of hands) who self-identified as interested in doing more science communication, which I think is a great thing. This shows scientists have bought into the importance of outreach and are looking for avenues to explore. A lot of these lessons about effective engagement of audiences are applicable in my work too. For me, the most striking thing was that respect for the people you’re trying to reach is key.
On Friday (February 17, 2017) Naomi Oreskes gave a plenary talk called “The Scientist as Sentinel” that touched on a lot of the ideas that were mentioned during the communicating science seminars. Oreskes is the author of the book Merchants of Doubt about the scientific “experts” brought in to shape public opinion and policy on everything from smoking to climate change. It’s a wonderful book, and, though it certainly filled me with righteous indignation, I would encourage everyone to read it. Oreskes’ talk was about the role that scientists can (and should be encouraged) to take in standing up for their science and themselves. She started off by saying that often scientists want there to be a bright line between science and policy, and as such they tend to want to “let the facts speak for themselves” because speaking up publicly about science dulls that bright line.
Oreskes talked about how their is a continuum of ways scientists can approach defending their work ranging from completely hands-off, leaving it to others to communicate with the public, all the way to the activist ideal, suggesting policy and perhaps even demonstrating (or getting arrested) in defense of the work. She advocated that scientists could seek middle ground, as a “responsible scientist” model of outreach.

The description of Oreskes talk in the program. Photo by me.
Oreskes made the comment that [with regards to climate change] what is rational is to be alarmed, and what is irrational is to be complacent. Scientists, who bask in the identity of being rational, can therefore identify the value in speaking up. She brought up the idea that climate change denial is not about facts, because, if it were, the alignment between a person’s political affiliation and their beliefs about climate change wouldn’t be so strong. When arguments aren’t about facts, they can’t be refuted with simply more facts. When it comes to scientifically controversial issues, the argument is often the same, if we deal with [insert issue here] it will lead to bigger government, and thus constriction of our freedoms. It isn’t a scientific controversy at all, but a clash of political ideologies. Scientists aren’t going to get very far bringing climate data to an economic and political ideology battle.
Oreskes put our current landscape for scientists speaking up against the historical backdrop of the scientists who spoke out against the use of nuclear weapons. Often, these were scientists who were involved in their creation. Her argument was that those scientists never lost scientific credibility for the act of taking a stand. Their science is still regarded with respect by their peers and the public. The same can be true for scientists who take a stand today. One of her closing thoughts was that scientists who have become the target of personal attacks were not attacked because they spoke out in public, instead they became public figures because they were attacked for their work. Ignoring the situation will not help or insulate scientists from the need to defend important work.
For me, Oreskes talk was one of the highlights of the conference, and I’m glad I was able to attend.
Of the rest of the sessions that I attended over the course of the conference there are two topics that stood out to me as particularly important (and about which there were several sessions each). The first is CRISPR, and the ethics, policy, and scientific progress being made with regards to human gene editing. The second was fake news and the distortion of facts. Both of these seemed like trends with regards to what people are concerned about and interested in.
From the CRISPR sessions, one of the main ideas that I took away is that if (as is currently recommended by the National Academies) human gene editing is only urged for “serious” health problems we need to define what counts as serious, and determine who gets to make that decision. If we are urging against changes that could be considered “enhancements” we need to find the line between treatment and enhancement, and, again, decide who will make that decision. If we’re looking to our government to make these policy decisions, it’s important to remember that, due to the separation of church and state federal scientific agencies (such as the Food and Drug Administration) don’t have the mandate to take religious beliefs into account when making decisions, despite the often religious-based concerns held by the public.
From the fake news sessions, what I walked away with was a sense that while it is a problem, there is reason to hope because fake news has always existed. Media has always been fragmented, rather than monolithic, and there have always been issues that Americans did not debate civilly. Fake news used to be found most often in the fringe – radio, newsletters, and in face-to-face conversations. The internet has changed the accessibility and spread of fake news. But even “traditional” outlets like television have been responsible for the spread of false ideas, like the fact that a majority of Americans believe that Sarah Palin uttered the words “I can see Russia from my house” when really it was Tina Fey, pretending to be Palin on Saturday Night Live. From all of this it may seem like people don’t care about or respect science, but they do. If you didn’t value science, you wouldn’t want to have facts or data on your side. Perhaps there is a way to tap into that trust in science.
Overall it was a conference that was very applicable to our current science communication landscape, and that left me with plenty to think about with regards to how I can be most effective in my job moving forward.
Note: I did not individually call out many of the speakers in the sessions I attended (though I did link to some and all can be found in the AAAS 2017 program). This is because, by and large, what I’ve written here is my synthesis of what I heard, sometimes combining several speakers and mostly put into my own words. I did not want to put responsibility for my interpretation of information on someone else unless I felt confident that my notes could accurately quote them. I do want to be very clear that these are not original ideas of mine but my interpretation of what others shared.
What I’m Reading: The Firebrand and the First Lady & Hidden Figures
The more I learn about and bear witness to the world, the more I’ve realized that my classroom education left out some aspects of history that give context to world and national events, and shape how I understand and interpret them. Reading is one of the best ways I’ve found to introduce missing perspectives and fill in gaps in my education.
Growing up I certainly had an awareness about the civil rights era–we learned about Rosa Parks, Martin Luther King Jr., and Malcolm X in school. But, even though I learned about these important people, there are so many others whose names I should also know, that I don’t. Pauli Murray and Katherine Johnson are just two of those names. Luckily, reading brought their stories into my world, and helped add depth to my knowledge about the various contributions of people of color to the United States during the civil rights era.
The Firebrand and The First Lady by Patricia Bell Scott
I learned about these two women by reading books that I think offered a lot of good information about US history and the role that women of color played in it: The Firebrand and the First Lady by Patricia Bell-Scott and Hidden Figures by Margot Lee Shetterly. Science writing and science history tend to comprise more of my reading list so Hidden Figures was in my conventional wheelhouse more so than the Firebrand and the First Lady, but both books were still quite different choices for me, being written by and about women of color. While I’m embarrassed by how little of my bookshelf came from or is about women and people of color, it is something that I can and am consciously fixing.
The Firebrand and the First Lady tells the story of the friendship between Pauli Murray and Eleanor Roosevelt. Murray was a lawyer, a civil rights and women’s rights activist, and the first black women to be ordained as an episcopal priest. Eleanor Roosevelt was the first lady of the United States from 1933-1945, US representative to the United Nations 1946-1953, and an important political figures in the women’s rights and civil rights movements. With neither woman alive to speak for themselves, the author draws heavily on the letters they wrote to each other.
Being able to see the letters they wrote to each other, especially when they disagreed, was amazing. It really was a snapshot from another time, where people with opposing views could find common ground and unite around a shared respect, treating each other with civility and thoughtfulness. It just struck me as sweet and sad that there was once a time when a young woman could reach out to a political figure and not just get a reply, but get true buy-in and a relationship that lasted the rest of their lives. I don’t think we currently live in such times, although this lovely piece by Jeanne Marie Laskas about how President Obama handled his mail, reading 10 letters a day from the public was a nice reminder about how important it is to have elected officials who hear you.
In telling the story of Murray and Roosevelt’s extraordinary friendship, the author gave an overview of the civil rights movement and the role that women played in it. But it was also an extremely American story, about how regular people built themselves up through education and hard work to leave an imprint on the world through the changes in policy and law that they helped bring about. The book left me not only knowing Murray’s name, but also with a profound respect for her.
I felt sympathy for Roosevelt, being a power broker but with limitations, and needing to figure out what she could do, what she should do, and how to pick which battles were the ones worth seeing through. She wasn’t able to do all that she wanted to, and yet she did so much more than most. But I was glad to see that Murray always held Roosevelt’s feet to the fire. In some ways, seeing Roosevelt’s responses felt like a master class in how to deal with criticism, and how there is always more that we can all do to help improve life for those around us. Being pushed to be better is a gift in many ways, but it’s also an endorsement of your own worth– that you’re worth improving.
Hidden Figures by Margot Lee Shetterly.
Hidden Figures is quite a bit more well known, now that it has been made into a box office-topping film. Despite there being a movie version, the book is certainly worth your time. It tells the story of the black women “computers” (in the literal sense of “people who do computations,” but really mathematicians and engineers) who worked at NASA during its formation and at the dawn of the space race. It’s been written and said by others that the fact that this story hasn’t been told before is amazing. I certainly am not the first person to notice that this is a trend, the contributions of women of color being erased from the history that gets handed down. I’m glad that this book is as popular as it is because it is bringing this bit of history to the forefront and giving the amazing women whose story the book tells the place in history that they deserve.
One of the important things about Hidden Figures that has been said in this article and elsewhere is that, while it might be about events that took place from the 1940-1960s, there are still trends and themes from then that echo through research institutions today. Certainly for women of color working in physics today there are still numerous barriers to success and discrimination that white women and women in other fields don’t encounter.
Ultimately, I recommend both of these books, they are beautifully written and offer a point of view that I found incredibly valuable for expanding my understanding of the role that women of color played in US history. That context is important for understanding the tumultuous political climate of the world today, and I’m grateful to the authors for telling the stories of these women.
A day in the clinic: shadowing a physician
Disclaimer: Speaking for myself as an individual in this post, not on behalf of my employer.
There is a lot to be gained from stepping out from behind your desk once in awhile. I work in the Dana-Farber Cancer Institute’s Division of Development and the Jimmy Fund. Our offices are down the road from the main Institute campus, which is a comprehensive cancer center. I’m fortunate that my responsibilities bring me to the main campus often, but many of my colleagues do not get such opportunities. To help keep our entire division connected to the Institute, every year we have a shadow day where the people who work to raise money to support the Institute get to shadow someone who works in a different role at the Institute for a morning.

Thumbs up for having a job you enjoy.
The shadow assignments can be anything– in the past, I’ve shadowed researchers and the leader of Dana-Farber’s gift shop. Other people have followed members of the community benefits program, patient resources, maintenance, etc. This year I had the opportunity to shadow a clinician as they saw patients.
It is such an intimate experience to sit in on someone’s appointment with their physician. To squeeze into the room with the patient and their family and listen as they detail their concerns and thoughts, looking for guidance and help. I was grateful (and somewhat shocked really) that so many patients welcomed my partner-for-the-day and me into their appointments. I’m not sure that, in their shoes, I could have been so gracious.
The patients’ graciousness was noteworthy, in part because these were cancer patients: people touched by one of humanity’s most daunting adversaries. Their uncertainty resonated and found uncertainty in me. Sure, I do know a bit about being a patient, but not a cancer patient. I know about cancer research, but from an outsider perspective–not that of physician or patient. This peering into a patient appointment was something new. I knew enough science and medicine to keep up with the conversation, and enough to be able to empathize with the patients, but truly it was an eye-opening experience.
In a morning of novel things, a few stood out to me. One was how quickly the physician was expected to switch from topic to topic. In the in-between moments when we weren’t in the examination rooms with the patients, the doctors darted around the hallways, conferring with the nurses here, with the radiologist reading the patient’s scans there, updating patient records, consulting notes,writing notes, or placing calls to other physicians. There really never was a “down” moment in the four hours that we were there.
For one of the patients that day, the nurse and the physician had different plans for how they intended to handle the patient’s unique situation (another disease on top of their cancer), and they had to devise a single game plan. Knowing Dana-Farber it was perhaps not surprising to see that all voices from the care team got heard, but it was still refreshing to witness.
Something else that struck me about the experience is actually a lesson I learned myself during my own health scare: while physicians are the experts, you need to keep track of your care plan and participate actively. Often patients or their families know more details and the context of the situation than the physician may remember off-hand, especially when the physician sees a lot of patients with similar diagnoses. The task-hopping required of these clinicians makes it impossible to remember all of the things you’ve discussed in prior appointments exactly without prompting sometimes. It’s not imprudent to jog their memory or ask them if they’re sure about something. You can and should question your doctors; if something doesn’t seem right to you, just be reasonable. Listen to their expertise, trust their evidence, but still make sure you’re bringing up your concerns.
It was also particularly interesting how quickly the physician had to change their approach as they went from patient to patient. The patients we saw that morning ran the gamut, and each was in a different stage of their cancer experience. There was optimism of a promising diagnosis alongside terminal cases where nothing else could be done. There were chronic patients and patients for whom the cancer was not their primary health concern. It was fascinating to watch the physician read the room and get a sense of how the patient and their family members were feeling and try to meet them where they were. As with all things, I think there were hits and misses, but, for the most part the personalization of each appointment was a really positive thing.
For me, because I write about forthcoming solutions in the form of therapies, it really felt like I was getting a sense of the meaning of the work. This is what it’s all about: trying to help the people that come for care. I write often about the type of cancer that the patients we saw actually have, so I’m very familiar with the drugs. It was striking to see patients feeling good on some of the newer medications, even in cases where they weren’t going to be cured and they knew it. Having a good quality of life in the time they have is really significant. You do the best you can with each unique situation, but to at least be able to offer patients the chance to feel better even if you’re not getting them that much more time still felt like a win of sorts. Maybe not the ultimate win, but not a dismal failure either.
I’m extremely grateful to have had the chance to see just a snippet of the work that Dana-Farber researchers and clinicians do. In development, it can sometimes feel like we’re not actually involved in what Dana-Farber does, because we’re just raising the money. The shadow day experience helped me to feel more connected to the fact that everything we do is about helping patients. It was a good reminder of why I chose to work in a non-profit and what drew me to this kind of science writing in the first place. I wanted to be an advocate and an ambassador for science, for a cause, and I can’t think of a better one than this.
Collateral Damage

My left knee directly after surgery accompanied by ice packs.
In January 2014, I fell crossing the street. In my defense, it was a damp day that felt like it could either rain or snow, and the streets were already slick with moisture. I was hurrying to cross while I still had the light, and, right as I was in the middle of the road, my right foot shot out from under me. I had slipped on the white paint of the crosswalk, essentially doing an unintended split. My left leg was behind me, and I landed on it, putting all of my weight on my left knee and winding up in a sitting position. The fall hurt, in the way that most falls do. I was scraped and bruised (but mostly embarrassed). But I got myself up, and continued on my way to work, thinking little of it in the days and weeks afterwards.
This fall was one of the signs I missed. Looking backward, it has become clear why I fell. To be fair, at the time, I didn’t know that I was walking around with a benign brain tumor altering my system of balance. The bruises on my knee were low priority compared to diagnosing and addressing my other symptoms, hearing loss and vertigo. Everything in my life became centered on the symptoms of the tumor – symptoms that wouldn’t be diagnosed until two months later.
As badly as the tumor damaged my ability to balance, the surgery to remove it made it worse, albeit temporarily. I needed physical therapy (vestibular rehab) to retrain my brain to balance, which helped me get back on my feet. While I was working on my balance, I noticed a nagging pain in my left knee. I shrugged it off as mere stiffness from having been inactive for so long while recovering. But it didn’t go away and hurt more as I became more active. In the following months, I would start to think that this knee injury was like my brain tumor’s last “screw you”– the final parting shot.
Fed up with being sick, I got good at ignoring the discomfort. I wanted so badly to feel like myself again and get back to my normal. The last thing I wanted was something else wrong with me that needed medical attention. So, even though I knew the pain in my knee wasn’t normal, I gritted my teeth and just dealt. It was nearly a year later before I realized my knee pain had gotten much worse. While I can be ostrich-like with my head in the sand when it comes to my health, the knee pain of spring 2015 was something I could no longer ignore.
I started with my primary care provider, who recommended an orthopedic specialist. I had pain in several different parts of my left knee: in the front near the patella (knee cap), along the inside of the joint, and towards the back. This variety of pain sources made it a little more difficult to pinpoint the problem, but I agreed to start with some physical therapy to see if that could help. The PT did help some of the pain, especially along the inside of the knee, which was diagnosed as pes anserine bursitis. Basically, the fluid-filled pad cushioning the bones of my knee was inflamed and tender. Even after the PT, there was still lingering pain in the knee, and it just didn’t feel right, so I asked the orthopedist for an MRI.

Knee all wrapped up in bandages a few days after the surgery.
The MRI showed a lateral tear in my meniscus. The meniscus is the rubbery cartilage disc that cushions the tibia (shin) from rubbing against the femur (thigh). Typically, meniscus tears are caused by forceful twisting of the knee– exactly what I did when crossing that street. Next to my tear was a bonus cyst, which was adding to the pain. The orthopedist and I concluded that, if physical therapy hadn’t helped enough, the only remaining option was surgery.
After what I’d been through with the brain tumor, I was hesitant to have another surgery. It was hard to be so dependent on other people after a procedure, and waking up from anesthesia was a horrible experience. Rationally, I knew the knee surgery wouldn’t be the same as the brain tumor surgery, but I still couldn’t get motivated to actually schedule it. Pain won out though, and I had to accept that I needed the surgery if things were going to get better. At 27, it didn’t make a lot of sense to resign myself to living with constant pain. I struggled going up and down stairs, couldn’t walk far distances, and running was completely out of the question.
I decided that the beginning of March made the most sense for when to have the surgery. It’s when Boston usually starts to thaw, so I would not likely have to contend with much snow. I also timed it between travel and social requirements, so I would have time to recover. My parents were able to take time off of work to come up to Boston to stay with me, which was particularly helpful; I’m pretty sure I would have started clawing at the walls if left alone during recovery. Of course the timing wasn’t great for work – but it’s never completely convenient to take two weeks off from your daily activities. There was a lot of emotion built into getting my knee fixed because of what I’d been through when I injured it, but I knew it was the right choice (and it was really the only option for feeling better).
The surgery itself was on March 1st, and went as smoothly as possible. I could have had it at a hospital in Boston, but it made more sense to go outside the city: it left the hospital for emergency cases, which is what they’re designed for, and moved my outpatient procedure to a facility that it was designed for. I suspected that the outpatient facility would be calmer and make for a more focused experience, which it was. I also didn’t want to be in the very same PACU that I’d had my brain tumor surgery experience in; I felt like that place would bring up memories and emotions that I didn’t want to relive.

Knee without the bandages, about a week after the surgery. You can see my surgeon’s initials where he signed my knee before the procedure.
It was all over in a couple of hours. I didn’t have nearly as much trouble waking up in the PACU this time, although I did get some momentary vertigo as I was coming to, which was scary given that I was still pretty out of it. Mercifully, it passed quickly and things went back to normal. Within a couple hours, I was dressed and able to get in the car to go home. Once home, it was couch and Netflix. I was only on the crutches they gave me for two days, and, after that, I started walking around on my own.
I’m going to need physical therapy, but I can already tell that the pain from the torn meniscus is gone. Not that there’s no pain–recovery can be tough and there is still a little of the bursitis that I had before–but I can tell the nagging, limiting pain is gone. After compensating for one weak knee with the other strong leg, I now have to regain strength and steadiness and equivalence between both. Having spent most of my life with no health issues, and now having undergone two surgeries in two years, I definitely have a different perspective on what not feeling well means. I am optimistic that, finally, I’ll be able to feel better. I will get back the way I was before the brain tumor and balance problems, before the knee pain. It’s an opportunity that I know many people who endure similar illnesses and injuries don’t get – the chance to go back to full health.
The View from the Stage: My Story Collider Experience
I have very limited experience being on stage. I’ve never been an “all eyes on me” type of person. I rarely, if ever, give talks or speeches for work, and, when it came to theater productions growing up, I was happier in the lighting booth and running around backstage. My on-stage experience amounts to one disastrous talent show where I was supposed to do a ballet routine, spun around once, burst into tears and stood on stage crying for the remaining three minutes of the song. Afterwards kind adults kept coming up to me telling me I was great, and, even at the age of six, I was the person that replied, “no I didn’t, weren’t you watching?!” My only other performance remains my third grade school play, which was called “Project Rescue: Save the Earth” and was about recycling. I played a raccoon. I had no lines.
Given this tremendous wealth of stage experience, I recently figured it would be a great idea to get up on stage in front of a theater full of strangers and tell them all about one of the most traumatic events in my life. Why not?
In the Fall of 2015, I volunteered to tell the story of how I diagnosed my own benign brain tumor at the Story Collider. I’ve been a huge fan of the Story Collider since I met the show’s co-founder Ben Lillie in 2013 and was introduced to the concept. The Story Collider is a live show where people get on stage and tell the audience a true story about science. With this as the founding concept, the stories cover nearly everything. Each show consists of five storytellers who take the stage for about 10 minutes each. Sometimes the stories are funny, sometimes heartrendingly tragic, but they’re always in some way about how science impacted the teller’s life. The Story Collider also has a weekly podcast, where they publish one of the stories from the live shows.
As the dust was settling from the entire brain tumor episode (around the fall of 2014), I started thinking that eventually the saga would make a great Story Collider tale. I wasn’t particularly ready then to get on stage and open myself up in that way, but I knew that it was something that I wanted to do in the near future. I think there is a lot of power in taking control of your own story and telling it your own way. I also feel like my story can help people by sharing what I went through and maybe even helping someone avoid the same mistakes I made– that’s why I wrote about it after it happened and why I wanted to tell the story publicly.
It took until the summer of 2015 before I felt ready to take the stage, I had been feeling kind of stagnant in the science communication side of my life and thought that getting involved in Story Collider could be a good way to shake myself out of it. Ben connected me with the Boston show’s producers Ari Daniel and Christine Gentry, and together we decided that the story would be a good fit for the December show (there was a Fall show for the NASW conference that I was not brave enough to do. Strangers are one thing; professional peers are another – hats off to the daring souls who took the stage during that show!)
As I started working out what I wanted to say, I realized that I would have to focus on just a subset of the brain tumor ordeal. There are a lot of different angles I could take, but I decided that the part I wanted to concentrate on was what came before– the two years from when I started to feel sick to when I was diagnosed. I chose this time period for a few reasons: while I was seeing doctors and talking to others about my health, I was really in it alone, so a lot of the story is about what I was thinking and feeling. I wanted to talk about the doctor who got it wrong and the one who got it right. I wanted to talk about my regrets in those two years. Perhaps the most interesting thing about the entire episode is when I diagnosed myself correctly long before any medical providers did.
Brain tumors are rare, but my tumor was a vestibular schwannoma, which is really rare: 2,000 – 3,000 yearly U.S. cases. Among primary brain tumors (those that arise from the tissues in the brain) the majority are non-malignant (like mine) but with more than 100 distinct types of brain and central nervous system tumors it’s a very tiny pie, being carved up into 100 even smaller little sections. Hitting the bulls eye, and getting the diagnosis EXACTLY right, as a joke, my first time out of the gate is incredible. It’s not that I’m particularly smart or anything, I’m just an informed person who got lucky – but still – hell of a thing, right?
The topic that I was most nervous about covering was my doctors. I know there is a ton of snark out there about how doctors are well trained, and making a diagnosis isn’t as easy as just going to google, and too often patients come to their doctors with whacked out ideas about what they might have. I get that, and I respect medicine as a field, and I know that doctors go through a tremendous amount to get trained, certified, and practice. But doctors are still just people. Highly trained people, with incredibly specialized knowledge, but still, just people. People can make mistakes. People can be dismissive. People can be cruel, and cold. Doctors aren’t above any of this– no one is. But doctors hold their patients lives in their hands, and, when you’re counting on someone to have the expertise necessary to help you, and you trust that they do, being dismissed, when you’re right, is a terrible thing to experience.
I wanted to tell how the medical system failed me at points, but I didn’t want it to be mere doctor-bashing. Yes, I saw a doctor who missed what others with medical backgrounds have told me were textbook signs. But I also had an amazing doctor who understood the significance of my symptoms right away and advocated for me as her patient to get the best care. I also had an amazing surgical team that went above and beyond to take care of me. (I still feel that I owe my surgeon her vacation days back; yes, the hospital’s only specialist in my type of tumor left her vacation to come back and treat me.) As with all things, there was good and bad. I wanted to make sure both the doctor who dismissed me, and the doctor who pushed me to get diagnosed properly appeared in my story. The choices made by these two people and how they treated me as their patient drastically and permanently changed my life.
I’ll never know whether the surgeons could have used a different surgical approach that would have saved my hearing if only I had been diagnosed by that first doctor. By the time I knew what I was dealing with, the tumor was so large that, for my safety, a hearing-sparing option was out of the question. If only we had seen it sooner, would it have been small enough? I think it probably wouldn’t have, and I’d have lost my hearing either way, but I’ll never fully know. If my primary care doctor hadn’t been so adamant about getting me diagnosed immediately after she saw me, would I have become unable to move my face? That was a real possibility, and was the reason the surgeons opted to do the procedure right away. If these two doctors had made different decisions, how would my life be different now? I think about that a lot.
That’s the story about science that I wanted to tell at the Story Collider. It’s the story of how I struggled with myself to find the truth that I didn’t want to be real among all of these conflicting forces giving me different information. Dissecting what happened to me in this way is something that I had avoided doing for a long time, but writing my script felt like such a rewarding exercise. It was good to turn all of these things over in my mind, and I think forcing myself to tease out my feelings about the whole thing helped me to come to a more secure sense of resolution about what happened. Sharing the story with a live audience was just the icing on top.
The show was in December 2015, and I shared the stage with four other storytellers: Kaća Bradonjić, Kamau Hashim, Meg Rosenburg, and Abhishek Shah. It was an absolute pleasure to share this experience with them; their stories were all amazing. The theme of the show was “The Art of Losing,” which I thought fit all five stories together perfectly. It was a total rush to take the stage. I feel like my emotions and adrenaline were running so high I don’t really remember the experience. It was like time warping. I just stepped up to the microphone and started talking, and then it was over and people were clapping.
Here is the audio recording of my performance at the show:
Overall it was a great experience for me, and I hope that people enjoy listening to my story. If you aren’t familiar with the Story Collider, I encourage you to check it out. It remains one of my absolute favorite means of science communication. They have live shows in an expanding number of cities, and there is always the weekly podcast – so plenty of opportunities to hear true stories about science.
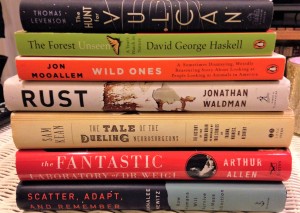
What I’m Reading: Two Years’ Worth
It’s been a long time since I’ve reviewed any books on this blog, but that doesn’t mean I stopped reading. I have devoured quite a bit of non-fiction in the past two years with occasional forays into fiction. I want to share with you a list of the things I’ve been reading lately. Even though I read them all in the last two years, some of these books have been out for a long time, while some are more recently published. I don’t really have a set way of figuring out what I’m going to read; it really comes down to whatever attracts my attention. If it’s listed here, I enjoyed it in some capacity, but I certainly have my favorites that stood out to me more than others.
In non-fiction, I don’t think I could possibly say enough flattering things about Rust by Jonathan Waldman. I absolutely loved this book, but I was surprised by how much there is to say about a topic like rust. It’s an incredibly compelling story, and I learned a lot not only about the science of rust and it’s history but also about the problems rust poses in the United States today in terms of infrastructure. Having gone to college just steps away from the abandoned Bethlehem Steel mill, I also got a kick out of his adventures exploring the hulking ruins I’m so familiar with. I thoroughly enjoyed the book, and completely recommend it for anyone who likes non-fiction and just learning about a new topic. I was also very impressed by The Forest Unseen by David George Haskell. It chronicles an interesting exercise in which the author watches and records what happens in a single patch of land for an entire year. I thought it was unique and beautifully written.
I read a lot of science history books; it’s probably the genre I find myself pulled toward the most. In this realm, I absolutely loved The Girls of Atomic City by Denise Kiernan; it certainly tells a side of the development of the atomic bomb that you don’t often see. I also read three books by Sam Kean, and enjoyed them all. He does an amazing job of putting scientific topics into current and historical context. I find his books consistently entertaining. They’re full of fun narrative bits that bring the topics to life. I also have to specifically mention The Fantastic Laboratory of Dr. Weigl by Arthur Allen. I was completely fascinated by this account of research using body lice during World War II, it was an aspect of the war that I’d never heard anything about. I was sharing fun facts about body lice with friends, family, and acquaintances for some time after I finished it. I think people probably got tired of hearing me say, “did you know….” and having the second half have to do with lice.
I haven’t listed below all of the fiction books I read, but one highlight was discovering Michael Crichton for books aside from Jurassic Park. I really enjoyed Sphere in particular. I also spent the better part of the two years listening to every Harry Potter audiobook. Somehow I managed to get to my mid-twenties never having read a single Harry Potter book– better late than never. It probably goes without saying that I loved them. I really enjoyed having them read to me by listening to the audiobooks; hearing everything pronounced in a British accent really puts the books over the top. I also read a collection of short stories by H.P. Lovecraft, and the Complete Sherlock Holmes by Sir Arthur Conan Doyle. I was also a big fan of The Circle by Dave Eggers, although I have to admit I found the ideas it presents for our future quite frightening (like, haul up in a shack in the woods frightening). Which is the point, I think it’s supposed to do that. Or at least make us think more critically about how much we share online, why we share it, and which entities we allow to own our information.
I go back and forth between reading paper books and using a Nook. In general, I tend to buy my non-fiction books as books because I truly wouldn’t mind living in a library (which seems possible in a small apartment sometimes). I usually don’t buy paper books for fiction, but I’ve read some that were borrowed. For fiction I typically rely on my e-reader, especially for collections and murder mysteries, which I’d say are my main guilty pleasure.
So, if you’re interesting in checking out some of the books that I’ve enjoyed here’s my list:
The Billion-Dollar Molecule – Barry Werth
Bossypants – Tina Fey
The Case of the Dueling Neuroscientists – Sam Kean
The Disappearing Spoon – Sam Kean
Driving Mr. Albert – Michael Paterniti
Empires of Light – Jill Jonnes
The Fantastic Laboratory of Dr. Weigl – Arthur Allen
The Forest Unseen – David George Haskell
The Ghost Map – Steven Johnson
The Girls of Atomic City – Denise Kiernan
The Half Life of Facts – Samuel Arbesman
The Hunt for Vulcan – Thomas Levenson
I Was Told There’d Be Cake – Sloane Crosley
Infinitesimal – Amir Alexander
Into the Wild – Jon Krakauer
Longitude – Dava Sorbel
The Map Thief – Michael Blanding
Merchants of Doubt – Naomi Oreskes & Erik M. Conway
On the Move – Oliver Sacks
Scatter, Adapt, and Remember – Annalee Newitz
The Science of Harry Potter – Roger Highfield
The Secret History of Wonder Woman – Jill Lepore
The Skeleton Crew – Deborah Halber
Soul Made Flesh – Carl Zimmer
Thunderstruck – Erik Larson
Rust – Jonathan Waldman
The Violinist’s Thumb – Sam Kean
The Water Book – Alok Jha
Wild Ones – Jon Mooallem
Yes Please – Amy Poehler
10% Happier – Dan Harris
I also just want to mention that I wasn’t asked by any of the authors or publishers of the books listed above to review them or say nice things. No compensation, I just liked them and you might too.
Lost and Found in the Healthcare System
When you’re a patient in a hospital, you don’t need shoes. You’re not on your feet much, and they’ve got you covered with socks that have little white nubs on the bottom to keep you from slipping. This is why I didn’t notice that my shoes were missing until several days (I didn’t keep track of time very well ) into my hospital stay.
I was in a hospital for surgery to remove an acoustic neuroma (also called a vestibular schwannoma) that was growing on the eighth cerebral nerve running from my brain to my right ear. I’d checked into the hospital unexpectedly. I’d woken up that morning with increased symptoms and had gone to see my doctor straight from work. She recommended surgery the next morning, and wanted me to check into the hospital immediately. She told me to just walk to the emergency department, which was right across the street from her office – in fact for several blocks the area is nothing but hospitals and medical buildings. I walked in wearing my work clothes and a pair of black leather riding boots, and explained who I was and why I was there.
The first few hours after I was admitted were chaotic. There had been a terrible fire in Boston that day. Two firefighters lost their lives, and the emergency department at the hospital where I was treated received several patients from the scene. Since my surgery was unscheduled and my arrival unexpected, no one had clear instructions about where I was supposed to go.
As a patient, you have to belong to someone. A doctor has to say, “I’m responsible for this person”. This is the doctor who signs the forms, and at the end of the day is ultimately in charge of your care. My problem wasn’t that no one claimed me, it was that too many doctors claimed me. I had a doctor from the emergency department, a doctor for my ear, a doctor for my brain, and my primary care doctor attached to my case. There were conflicting stories about where I should be, so I was shuffled around a lot. The problem was that I didn’t fit neatly into one of the categories that medical specialties are divided into. I wasn’t just an unexpected arrival, I also wasn’t an easy to assign case. This meant that the hospital staff who were giving me instructions were themselves receiving conflicting instructions.
In the emergency department I was told I needed to be admitted in a building across the street. I offered to walk (according to Google Maps it’s just five minutes on foot), but was told that wasn’t allowed and had to be transported by ambulance. It probably goes without saying that I felt ridiculous. Once there I was told I actually needed to be in a different building on the side of the street I started on. Again, I wasn’t allowed to walk there, so that meant another ambulance ride. Once I arrived in the right building, I was assigned a room but was taken down for several hours to the imaging department. Finally, I arrived back to the room where I’d spend the night before the surgery. Somewhere along the route, I removed my boots in exchange for the slipper socks. By the time I settled into one place for the night, with 12 hours of neuro-surgery looming ahead of me, getting a hug from my Mom was far more important than the boots. I’d forgotten all about them.
After the surgery, I wasn’t in any sort of condition where I could think about shoes. I spent an entire day in surgery, and another lost in the fog of trying to wake up post-anesthesia. The type of tumor I had affected my balance, so walking was a struggle. A slow, plodding lap of the hallway outside my room, propped up by friends and family was all I could manage. After a few days, I started to pull myself together and remembered the belongings I’d had with me when I arrived at the hospital. My work clothes, my backpack, my grey wool pea coat, my boots. My family assured me they had everything, but when they went to show me, the clothes, bag and coat were there – but no boots. Somewhere in the shuffle, my boots had gotten lost.
For inanimate objects, I relate a little too much to my boots. I was never lost per se, but as a patient if your condition straddles medical specialties you can feel passed around. People are certain you belong to someone, somewhere, they just aren’t exactly sure where that is.
Every time I talk about how I had a brain tumor, I feel guilty. Guilty because that’s not quite accurate, and the science communicator in me can’t help but cringe. An acoustic neuroma grows from the nerve sheath cells that coat the eighth cerebral nerve, which controls your hearing. My tumor was in my inner ear – affecting both my hearing and my sense of balance. To classify my tumor as a brain tumor seemed off to me, after all it wasn’t growing from the cells that make up the brain itself. Yet, it was right next to my brain. Sticking to my brain, in fact. Sticking to my brain in such a way that hours of surgery were needed to get my grey matter to finally relinquish it. It was certainly brain surgery, but it wasn’t just a brain tumor. It was in my inner ear growing on the nerve. This is why I didn’t just have one surgeon, I had two (well, many people were in the operating room). One of my surgeons was a specialist in skull base neuro-surgery for the brain and one was an ear, nose, and throat surgeon for the inner ear. I was very lucky to have both of these doctors on my team.
As much as it was my medical team, I certainly wasn’t the one steering the ship that day. Since I was in an anesthesia induced stupor I wasn’t the team captain – so then who was? Two surgeons of equal standing, each with a different medical specialty, each with their own purpose for being there. Who was in charge? Luckily, my doctors have worked as partners for a while and there were no power struggles over my care, but it did come into question while I was recovering. Whose patient was I? Where did I belong?
The hospital floors were broken up by medical specialty. Did I belong on the neuro floor with the stroke patients? Or did I belong on the ear, nose, and throat floor with the patients having surgery for a cochlear implant? Where was I supposed to be? In the end, the hospital split the difference. My ear, nose, and throat surgeon became the primary on my case, but I spent my time recovering on the neuro floor. They sorted it out, and carved out a niche for me to belong, but the lines weren’t clear. I didn’t fit into the boxes our current system for dividing medical specialties silo patients into.
My boots didn’t fit either. We found out that the reason my boots were lost was because they didn’t fit in the bag they’d given me for my personal belongings. We had everything that had made it into the bag, but the boots had been unintentionally abandoned. When you don’t fit in the box, or the bag, assigned to you, your choices can be limited. You run the risk of slipping through the cracks. You can try to squeeze and jam your way into the appropriate container, but it won’t meet all of your needs. You can try to break out of the box, but you might get left behind. The human body works as a unit. Conditions like mine have effects on multiple systems, and don’t fit easily into a category. Special attention is required to make sure that patients who don’t meet the definitions make it to the right destination, and receive the right care.
Ultimately, the hospital lost and found tracked down my boots and delivered them back to me. They figured out to whom, and where they belonged. With me too, the staff sorted out to whom, and where I belonged. I received excellent care, and all of the support I needed for the effects the tumor had on my ear and hearing and the effects it had on my brain and balance. The whole experience left me wondering though, if we can’t do better than the lost and found? I’m not about to suggest ways to overhaul our healthcare system, because I don’t have any, but if I’d had more than one bag for my belongings (or maybe no bags at all) I might not have lost the boots in the first place.
What I’m Reading: Toms River
It’s been a long time since I’ve shared thoughts about anything that I’ve read. Not that I’ve stopped reading of course, in the past year I’ve made my way through many non-fiction science books that I’ve enjoyed but haven’t written about. I was on a blogging hiatus, but now that I have free time courtesy of the things detailed in this post, I want to rebrand my book review series. I’m not sure book review is accurate to describe the type of posts I write. While I share my opinions, I almost never write about books I didn’t enjoy and try to avoid negative comments. I do this because if I’m going to write a post I want it to be about something I’m excited about and enjoyed rather than something I disliked. Thus, I feel calling these posts What I’m Reading is better than Book Reviews. As always, if I’ve been asked to read a book by the author or publisher I’ll let you know, though nearly all the books I write about are chosen because they peaked my interest. Even with a new name, I hope people will still be encouraged to check out the books featured in this series.
When I’m reading non-fiction I gauge the success of the story by how quickly I finish reading it. Are the things on my to-do list falling by the wayside because I need to know what happens next? Am I so engaged that nearly 500 pages can be consumed within a few days, or are the pages trickling by as they lull me to sleep each night? Is the book so compelling that even the most technical details are devoured alongside the more narrative elements of the story? To cross the line from “I liked it” to “I loved it” a book needs to meet these criteria. I loved Toms River by Dan Fagin.
 In addition to being the name of Fagin’s Pulitzer Prize winning book, Toms River is the name of a town in New Jersey. I grew up in New Jersey in the 1990s and 2000s – just young enough to know that Toms River had a stigma attached to it, but not old enough to read the papers or understand why. When I found out Fagin was writing a book about the New Jersey town and it’s epic pollution problem, I was intrigued and quite frankly a little shocked by how little I knew about the environmental disaster that had taken place in my own home state.
In addition to being the name of Fagin’s Pulitzer Prize winning book, Toms River is the name of a town in New Jersey. I grew up in New Jersey in the 1990s and 2000s – just young enough to know that Toms River had a stigma attached to it, but not old enough to read the papers or understand why. When I found out Fagin was writing a book about the New Jersey town and it’s epic pollution problem, I was intrigued and quite frankly a little shocked by how little I knew about the environmental disaster that had taken place in my own home state.
As far as states go, New Jersey doesn’t exactly have a glimmering reputation. Since it’s not enough to have to contend with pop culture stereotypes like Jersey Shore or the Sopranos, we also have our fair share of government corruption and industrial pollution. Yet I feel protective of the “Garden State” (when you think of the pollution problems, the jokes just write themselves don’t they?) Where I grew up, on the boarder of Union and Morris counties, was the very picture of the idyllic New York City suburb. It was hard to imagine the state had a pollution problem when surrounded by the manicured perfection of sprawling lawns, parks, and golf courses. Yet, even as a kid, while I don’t remember any specific media coverage I remember the negativity, the impression that Toms River had problems. Until I picked up Fagin’s book, that was really all I knew about it.
While the details of the environmental disaster that played out in Toms River over the course of 50 years may have eluded me growing up I was aware of New Jersey’s distinction as the state with most Superfund sites. On their website the Environmental Protection Agency describes Superfund sites as:
“An uncontrolled or abandoned place where hazardous waste is located, possibly affecting local ecosystems or people.”
The government started designating Superfund sites after the Love Canal case in which toxic chemicals located beneath homes and an elementary school in Nigara Falls, NY started causing health problems in 1978. Toms River made it onto the list in 1983 thanks to the Ciba-Geigy factory, a 1,400 acre site where the chemical company manufactured primarily dyes, but also resins and epoxy. The company dumped waste products from the manufacturing process contaminated with toxic chemicals on the factory property, into the nearby river, and into the Atlantic Ocean from the time the factory was established in the 1950s. Toms River is a beach community, and the toxic waste easily seeped through the porous sandy soil to contaminate the ground water in the area. The groundwater cleanup started in 1996, when I was eight which is why I missed out on the majority of the drama.
Fagin’s book starts out by getting into the history of dye manufacturing. It doesn’t really sound like a topic that would be captivating, but I was fascinated by the backstory behind major chemical companies and how dye became a big business. Tracing the various companies through their founding, expansions, closures, consolidations, and mergers with clarity is a difficult task, and Toms River does it skillfully. I was hooked from the very beginning and as the story developed from the discovery of the chemical compounds used in dye manufacturing through the events that led Ciba-Geigy to open their plant in Toms River I found myself more and more impressed at how sucked into the story I became.
There is a turning point in the middle of the book where the story starts to shift from explaining how the pollution got into the water in Toms River, to explaining the affects of that pollution on the town’s residents namely the rise of a pediatric cancer cluster. I may be slightly biased in how interesting I find cancer epidemiology since I do write about cancer research for a living but I feel like Toms River handles an incredibly complex science with a perfect amount of nuance and explanation. The book even gets into the nitty gritty of experimental design without making me want to skip ahead to just find out the results. The intricacies of the studies needed to prove an environmentally caused cancer cluster became the drama for a big section of the book.
Woven throughout the book are the stories of the people involved from the first dye discovery through the operation of the factory all the way to the legal battle that sprung up once the cancer cluster was discovered. Generally I’d call the human element the narrative aspect of the story, the thing that drives the story forward, but that doesn’t really feel appropriate in this case. The entire thing is a compelling narrative. Still, Fagin does a wonderful job of injecting the story with the personal experiences of the people who lived it. The book culminates with settlement of the legal case regarding the Toms River pollution, and the scientific findings from the studies undertaken to prove that the cancer cluster had an environmental cause. These parts of the story are explained through the impact they had on the families of children with cancer and thus resonate deeply.
I really loved Toms River from start to finish, and recommend it for anyone regardless of your background knowledge or interest in science or environmental issues. It is just a fascinating story, told extremely well.